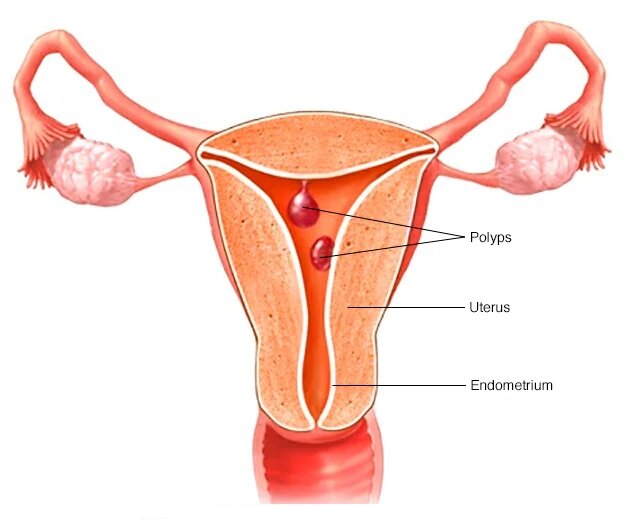
Uterine Polyps
Uterine polyps are abnormal growths on the inside lining of the uterus (the endometrium). These outgrowths are usually less than 1 cm in diameter. They are also sometimes called endometrial polyps.
The stalk of the polyp (or pedicle) is usually short, but sometimes it grows long enough for the polyp to project from the cervix (the lower opening of the womb). Uterine polyps are common and there can be more than one polyp in the uterine cavity. Sometimes small sub mucosal fibroids grow on a stalk and present as uterine polyps.
Polyps are prone to bleeding and large polyps can contribute to infertility and miscarriage. Uterine polyps can develop in pre- or post-menopausal women. Very rarely, polyps can be cancerous.
For comprehensive care, including options like Uterine Fibroid treatment in Mumbai/Fibroid removal Surgery, consult with specialists like Dr Anshumala Kulkarni, who can provide expert diagnosis and treatment plans.
Symptoms:
Many women who have uterine polyps show no symptoms at all. In others, one or more of the following symptoms may be present:
Irregular menstrual bleeding, such as bleeding of varying amounts and at frequent and unpredictable intervals
Bleeding between menstrual periods
Excessively heavy menstrual periods
Abnormal vaginal discharge
Vaginal bleeding after menopause
Cause
Uterine polyps occur when cells of the uterine lining (the endometrium) multiple number of times. As this happens, lumps are formed. These lumps often resemble hanging sacs or mushrooms made of tissue. Polyps can be few or numerous, and some people might only have one. Some research shows that oestrogen plays an important role in the formation of polyps, but it’s not yet clear how.
Some people are more likely than others to develop uterine polyps. They are most common in people who are peri-menopausal and postmenopausal. Obesity also makes people significantly more likely to develop polyps.
Prevalence:
Uterine polyps are very common. Up to 3 in 10 people may have them at some point in their lives, but fewer than 1 in 100 people develop polyps before age 30. They occur most commonly leading up to and after menopause. Small polyps may cause no symptoms at all and can go away on their own. In other cases, untreated polyps may cause symptoms that affect quality of life and can carry a small chance of becoming cancerous.
Diagnosis:
Often the following procedures are done to diagnose polyps-
Hysteroscopy – a procedure where a thin telescope like instrument is inserted into the uterine cavity allowing the surgeon to look inside the uterus.
Ultrasound – Thickened fold of the lining of uterus in younger women who are still having menstrual periods may be misinterpreted as polyps. For accurate diagnosis hysteroscopy may be needed.
Hystosalpingography – a procedure in which x-ray of uterus is taken after filling it with a dye.
It is important that a tissue sample from the polyp is sent for biopsy to rule out cancer.
Treatment:
Small uterine polyps can go away on their own without treatment. If they give symptoms they may be treated as follows:-
Medications: Hormonal medications are sometimes prescribed to treat the symptoms of uterine polyps. These include Gonadotropin Releasing Hormone (GnRH) agonists, which block the body’s production of certain hormones
Non-invasive surgery: Small polyps can be removed with a process called hysteroscopic excision. About 7 in 10 people with small polyps (<1cm) found their symptoms significantly improved after this procedure.
Lifestyle Changes: Research on this is still unclear, but weight loss may improve the prognosis of people who are diagnosed with both uterine polyps and obesity.
Prognosis/Future:
Uterine polyps, once removed, can recur. It’s possible that you might need to undergo treatment more than once if you experience recurrent uterine polyps. If the polyps are found to contain precancerous or cancerous cells, a hysterectomy (removal of the uterus) may become necessary.
Don’t let uterine polyps or fibroids impact your quality of life. Get a thorough diagnosis and explore surgical options for fibroids with Dr. Anshumala Kulkarni. Schedule your appointment in Mumbai for expert care and compassionate support.
