Uterine / Vaginal Prolapse
A uterine/vaginal prolapse is a dropping of your vagina from its normal location in the body. Vagina is one of several organs that rest in the pelvic area of your body. These organs are held in place by muscles and other tissue. These muscles come together to create a support structure. Throughout your life, this support structure can start to weaken. This can happen for a variety of reasons, but the result is a sagging of your organs. When your organs sag or droop out of their normal position, this is called a prolapse.
If you are facing uterine prolapse and considering treatment options, including Uterine Prolapse or Vaginal Prolapse Treatment, uterine prolapse treatment by robotic surgery offers a promising solution. Consult with a skilled and experienced robotic surgeon, like Dr Anshumala Shukla-Kulkarni, to determine if this approach is suitable for your specific condition.
Types of Prolapse:
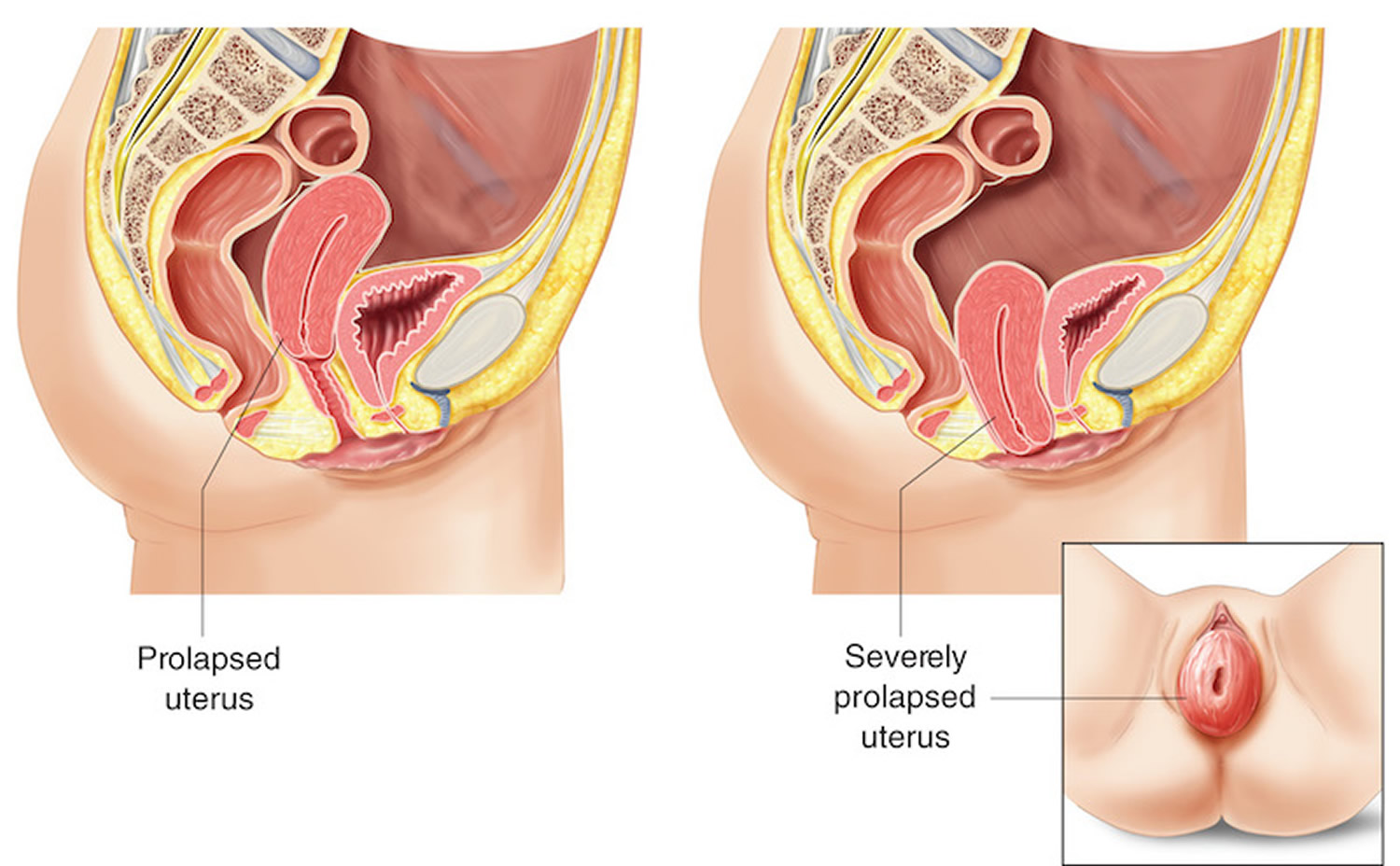
Prolapses can be small or complete.
A small prolapse is with just a little movement also known as incomplete.
A bigger (complete) prolapse is one where the organ has shifted significantly out of its normal place. It is a very severe condition in which organ may stick out of the body.
The different types of pelvic organ prolapse can include:
Vaginal vault prolapse – The top of the vagina (known as the “vaginal vault”) droops down into the vaginal canal. This usually occurs in women who have had a hysterectomy (removal of the uterus).
Uterine prolapse: The uterus bulges or slips into the vagina, sometimes so far that it comes out of the vaginal opening.
Cystocele: The bladder drops into the vagina.
Urethrocele: The urethra (the tube that carries urine away from the bladder) bulges into the vagina. A cystocele and urethrocele are often found together.
Rectocele: The rectum bulges into or out of the vagina.
Enterocele: The small intestine bulges against the back wall of the vagina. An enterocele and vaginal vault prolapse often occur together.
Symptoms:
Sometimes there may be no symptoms, if you do experience symptoms, they can include:
A feeling of fullness, heaviness or pain in the pelvic area(it may feel like sitting on a small ball)
Lower back pain.
Bulging in the vagina.
Organs slipping out of the vagina.
Leakage of urine (urinary incontinence).
Bladder infections.
Difficulty having a bowel movement.
Problems with sexual intercourse.
Difficulty walking
Causes of Prolapse:
Prolapse happens when vaginal childbirth or other conditions weaken the muscles and tissues of the pelvic floor so they can no longer support the weight of the uterus. It can happen as a result of:
Childbirth – with normal or complicated delivery through the vagina
Surgery – A procedure like a hysterectomy,radiation treatment in the pelvic area, could cause a prolapse.
Menopause – When your body doesn’t make as much estrogen as before, those pelvic muscles can become weak and a prolapse can develop.
Aging
Extreme physical activity or lifting of heavy objects – this may weaken your pelvic muscles and allow your organs to sag out of position.
Genetic factor
Lifestyle factors like being overweight, straining to have a bowel movement, having a chronic cough (such as in smokers or people with asthma) may also cause prolapse.
Prevalence:
Diagnosis:
A diagnosis of uterine prolapse generally occurs during a pelvic exam.
During the pelvic exam your doctor is likely to ask you:
To bear down as if having a bowel movement. Bearing down can help your doctor assess how far the uterus has slipped into the vagina.
To tighten your pelvic muscles as if you’re stopping a stream of urine. This test checks the strength of your pelvic muscles.
Treatment:
Treatment depends on how weak the supporting structures around your uterus have become.
Self-care at home:
You can strengthen your pelvic muscles by performing Kegel exercises. Kegels is done by tightening your pelvic muscles, as if trying to stop the flow of urine. Your doctor will instruct you on the proper ways to isolate and exercise the muscles.
You should have a regular follow up visit where your doctor can check the progress of your muscle strength.
Medication:
Estrogen (a hormone) cream or suppository ovules or rings inserted into the vagina help in restoring the strength and vitality of tissues in the vagina. But estrogen is only for use in select postmenopausal women.
Surgery:
Depending on your age and whether you wish to become pregnant, surgery can repair the uterus or remove it. When indicated, and in severe cases, your uterus can be removed with a hysterectomy.
During the surgery, the surgeon can also correct the sagging of the vaginal walls, urethra, bladder, or rectum.
The surgery may be performed by an open abdominal procedure, through the vagina, or through small incisions in the abdomen or vagina with specialized instruments.
You need to follow-up according to your doctor’s advice.
Pessary:
Pessary is a supportive device that you wear in your vaginal canal to support the falling uterus. You can use this temporarily or permanently. They come in various shapes and sizes and must be fitted to you. If your prolapse is severe, a pessary may not work. Also, pessaries can be irritating inside your vagina and may cause a foul-smelling discharge.
It needs to be cleaned and checked by your doctor for the correct position and fit at regular intervals unless you are instructed on how to remove it and clean it yourself at home.
If you are experiencing uterine prolapse and seeking effective treatment options, robotic surgery can be a beneficial approach. Robotic surgery offers advanced techniques and precision in treating uterine prolapse. Uterine prolapse treatment by robotic surgery provides a safe and efficient solution for addressing the condition. For an appointment simply fill out the form or contact us at 93239 11554. For clinic directions click here.
